ERECTILE DYSFUNCTION OVERVIEW
This guide has been created to help you understand more about erectile dysfunction (ED), a condition that was previously known as impotence. It may also give you insight into other sexual difficulties that some patients experience, which can often feel challenging to talk about.
During your appointment, you may have had checks such as blood pressure, weight, and urine tests, as well as being asked to complete a short questionnaire. These simple steps provide valuable information to your clinician and help build a clearer picture of your overall health and condition.
You will then meet with a clinician to discuss your concerns in more detail. Talking openly about sexual health issues, although sometimes difficult for patients and their partners, is an important step toward receiving the right support.
Following this conversation, further investigations may be suggested, and personalised treatment or guidance will be offered to help manage your condition.
Please use this guide to help you understand more about erectile dysfunction.
It can also enable you to know more about some of the sexual difficulties that patients can suffer, such as erectile dysfunction (which used to be called impotence).
At your appointment you may have had your blood pressure, weight and urine test done and be asked to fill in a questionnaire. These will help the clinician understand more about your condition.
You will then see a clinician who will talk with you. Being able to talk about your problem will help them understand what help you need. We understand that this can be difficult for patients and sometimes their partners who have sexual difficulties. After talking together, some further tests may be done and help will be given.
One in ten men has an erection problem 80% may have an underlying illness (organic).
Many men have a combination of organic and psychological problems, but it is not ‘all in the mind’. It is important to check that if there is an illness it is known about and managed.
An erection happens usually as a result of a sexual thought which activates the nerve supply, blood flow and stiffening of the penis. There can be several things that cause this mechanism to fail, and working it out is like putting the pieces of a jigsaw together!
A lot of men ask us what their sex life will be like after prostate cancer treatment.
Will I be able to have sex after treatment for prostate cancer?
In reality, the answer to this is different for every man and depends on what treatment you’ve had, whether you’re feeling up to it, and whether you’ve hadany sexual problems in the past. It is common for men to have difficulty getting an erection but this can improve with time and treatment. Many men will be able to have sex again but it is likely to be quite different. Remember, you can have orgasms without having an erection or ejaculating. And sex doesn’t have to be about penetration. You could try different things like massage, mutual masturbation, oral sex, vibrators or dildos. And you can get treatment on the NHS to help with erections – like tablets or a vacuum pump.
Will sex feel different after treatment?
Yes, sex can feel quite different. You’ll still have feeling in your penis and you should be able to have an orgasm but it may not feel the same. If you’ve had surgery you won’t ejaculate when you orgasm, but you will still get the feeling of an orgasm. If you’ve had other treatments, including hormone therapy, you may notice that you produce less semen and your sexual desire may not be the same. Again, you should still be able to have an orgasm but it may feel
different.
Do the treatments for erection problems actually work?
There are a number of different treatments for erection problems, such as tablets, pellets, injections, pumps and implants and different treatments will work for different men. These are not always a ‘quick fix’, and you often have to stick with them or try different ones to see what works best for you. Research shows that men who try more treatments are more likely to find one that works. For some treatments you need to have a desire for sex (libido) but others, like pumps, injections and pellets will work without this.
Why is hormone therapy affecting the way I feel about sex?
Hormone therapy reduces or blocks the effect of the testosterone that gives you your sex drive. Not having a sex drive may make you feel less confident about your masculinity and physical changes such as putting on weight, hot flushes or breast swelling, may have the same effect. There are ways to tackle this. Try focusing on the things you like about yourself, do activities you are good at, or try something new.
Talking about a sexual problem can be helpful, especially if a partner (when there is one) also comes to the appointment.
Advice can be given to make things better. It takes blame off a particular person and helps to open up a way of talking to each other. Practical advice is given and ‘the practice’ is then done by you at home. It is not always available on the NHS.
Psychosexual therapy can be helpful used alongside drug treatments.
50% of patients with diabetes develop erection problems.
Poor control of diabetes can lead to damage of the nerve supply and reduction of blood flow to the penis. Worrying about your diabetes can also affect your sex life.
Erection problems can sometimes be the early signs of developing diabetes. It is one of the blood tests you will or have had done to check.
There are many types of surgery that can cause erection problems.
- Prostate removal
- Bowel surgery
- Pelvic surgery
Patients and partners may worry about starting to have sex again after surgery. Talk about this to the clinician as they may be able to support you by answering any of your worries.
After prostate surgery there can be improvement with erections over time either naturally or by using drugs/mechanical device regularly.
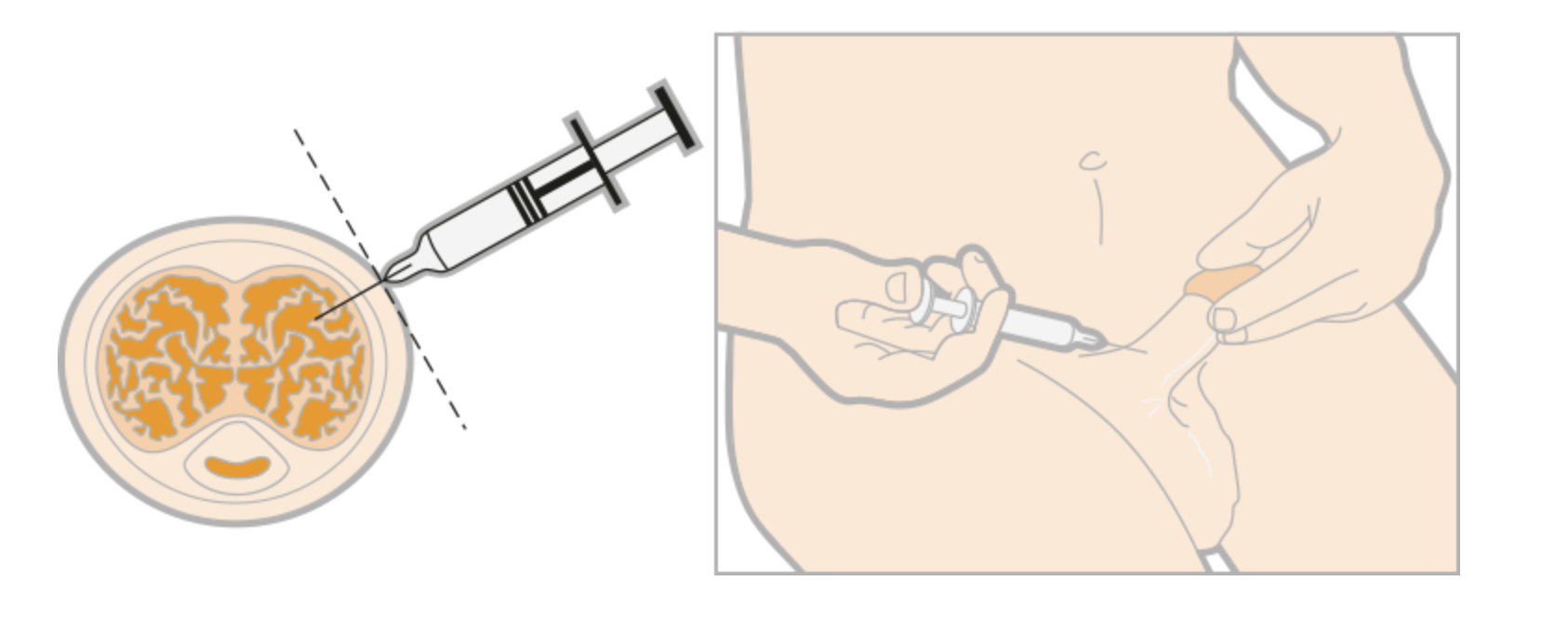
Caverject and Viridal Duo are the injections currently available.
It involves putting a very fine needle into the side of the penis (the shaft) and injecting a measured amount of the drug. It is important to start with a small amount of the drug and gradually increase the dose to get an erection to last as long as needed. Usually an hour is long enough and no longer than 4 hours!
(See PRIAPISM).
If you suffer from one of the following conditions you will be allowed one treatment a week using an NHS prescription:
- Prostate cancer
- Diabetes
- Severe pelvic injury
- Kidney failure treated by dialysis or transplant
- Multiple sclerosis
- Spina bifida
- Parkinson’s disease
- Poliomyelitis
- Spinal cord injury
- Single gene neurological disease
- Transurethral resection of prostate surgery
- Radical pelvic surgery
- Extreme distress
Tablets
All tablets need sexual stimulation to work. This may be by a partner or yourself (self stimulation). Viagra, Cialis and Levitra should NOT be used with nitrate drugs and certain other types of drugs.
The tablets are swallowed before sexual activity. They vary in how quickly and how well they work. The side effects of these tablets can differ between people.

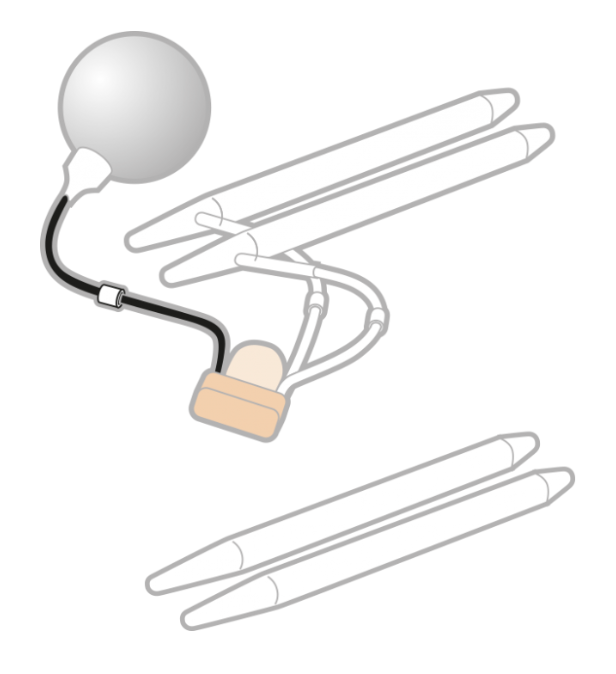
Several types are available such as ‘bendy rods’ or inflatable systems.
It involves an operation to remove some of the inside of the penis to put the implant in. This is usually considered only when all other treatments have failed. The money for the operation is not always available on the NHS. Not all hospitals have a surgeon who would be able to do this operation.
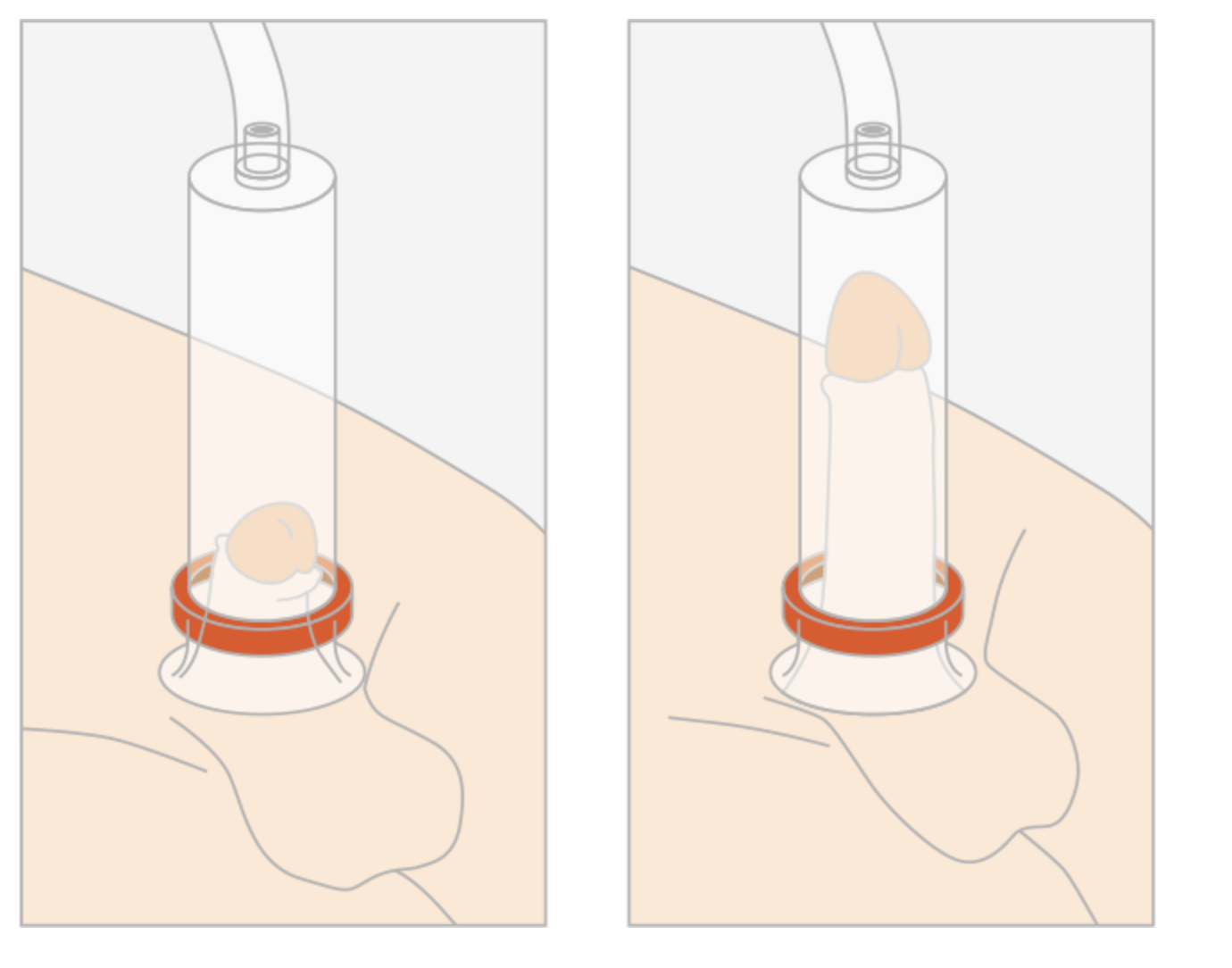
A vacuum device is a cylinder, which is usually plastic that you place over the penis.
Attached to it are a pump and a specially designed constriction ring. Using the pump removes air from the cylinder and the fall in pressure pulls blood into the penis like a sucking action. When the penis is stiff, the ring helps to hold the erection. To have intercourse the cylinder is removed leaving the ring in place. The ring should not be left on for more than 30 minutes.
These are also available on Schedule 2. There are many types available.
Keeping fit is important to prevent ill health.
It can also help prevent erectile dysfunction! We know that high blood pressure, diabetes, high fat levels in the blood and being overweight can make erection problems worse.
By taking regular exercise and eating a healthy diet we can try to stop these problems from happening, or getting worse.
Some tablets (such as those to help blood pressure) can have the unwanted side effect of causing sexual problems.
If this happens let the clinician know who prescribed them as there may be a different drug that can be prescribed to do the same job without these side effects. Some recreational drugs can make it difficult to have sex. This can include having too much alcohol!
Smoking can also make erectile dysfunction worse as it damages the vessels in the penis.
Often partners think they are not ‘fancied’ anymore in the relationship if there is an erection problem.
A common thought they have: ‘is my partner having an affair?‘ If not in a relationship men may worry that they will not get a partner if they cannot get an erection.
Talking with a partner as to how they feel is a good idea. Couples may stop kissing and cuddling if no erection happens and this can make things worse.
A history of heart disease does not mean you are unable to use treatments to help you get better erections.
How ‘stable’ your heart disease is should be considered. Having sex is no more stressful to the heart than other daily things such as walking one mile on the flat in twenty minutes or playing golf!
If you use nitrates (spray or tablets) to get rid of chest pain you MUST tell the person prescribing drugs for your erectile dysfunction. It may alter the treatment they would safely suggest.
Priapism is a prolonged painful erection.
If an erection lasts for more than four hours it is a medical emergency. It can cause permanent damage to the penis. Some treatments may increase the possibility of it happening, but it is a rare side effect.
If it should happen to you try these things to get the erection to go down:
- Engage in sexual activity (e.g. intercourse or self stimulation)
- Apply a bag of frozen peas (wrapped in a tea towel) to the penis
- Take a cold shower
- Run up and down a flight of stairs.
If they do not work go to your nearest Accident and Emergency.
Sexual Advice Association
College of Sexual and Relationship Therapists (COSRT)

I was honoured to receive a Developing Practice Award from the Queen’s Nursing Institute and the Men’s Health Forum, which supported me in creating this guide to improve awareness, education, and practical support for men’s health within our community.
Intimacy Guidance
Together we break stoma silence, openly discussing sex and intimacy.
Are you feeling sensitive about the changes an ostomy has brought to your body?
Even with these changes, you can still experience closeness, intimacy, and meaningful connections in your relationships.

LOOKING FOR SOMETHING ELSE?
Support IS JUST A CLICK AWAY
CLINIC LOCATIONS
Patients, please use the Carebit portal to book your appointment. Emails aren’t suitable for clinical advice, so I may not be able to respond with guidance.